What causes the body to generate the most common forms of head pain? How can we begin to sort out which type we may be experiencing and promote healing? Headache pain is often classified by recognizing how and why the body is generating pain.
Might the pain be related to nerves or chemicals reacting in the body? Or, perhaps, a headache is the result of a disease or situation that the body has encountered. How can the average person begin to decipher the pain? Basic classification techniques often include a division of primary and secondary headaches.
Understanding Primary and Secondary Headaches
Due to the infinite number of possible injuries, ailments, and diseases that one may encounter with one’s head, it can be rather difficult to concisely categorize all of the possible pain experiences. However, understanding the basics of primary and secondary headaches can help pain sufferers better navigate the road to healing.
Primary Headache
A primary headache refers to pain that is not a symptom of a disease, injury, or incident. According to the Mayo Clinic, “A primary headache is caused by overactivity of or problems with pain-sensitive structures in your head. A primary headache isn’t a symptom of an underlying disease.” While the reason for the pain may not be readily understood, overactivity within the head region is the direct source of the pain.
Secondary Headache
On the other hand, a secondary headache is viewed as a side effect of a disease or seemingly unrelated factor. It is secondary to the initial cause of the pain. A secondary headache does not develop without the presence of a separate issue somewhere in the body.
Tumors, aneurysms, and sinus pain are all examples of secondary headaches. Hangovers and ice cream headaches are also considered secondary. The secondary headache can be solved by removing the tumor or sinus blockage, or perhaps by consuming particular items with care. Let’s consider how a few of the most common headaches are generated by the body.

A Few Primary Headaches and What Causes Them
Pain associated with certain headache types remains a part of the mystery of medical knowledge, but it is rapidly gaining understanding. As technology reveals more and more of how the nervous system and brain send messages throughout the body, headache pain continues to become better understood. Individuals who suffer from one type of primary headache may also experience at least one other type of headache.
Since primary headaches are not generally the result of a particular disease or ailment, narrowing the source of the pain can sometimes be tricky. An exact reason for pain suffered by a patient may not always be readily identifiable. Yet, we can still take meaningful steps to minimize and alleviate headache pain.
Tension, migraine, and cluster headaches rest at the top of most listings for common headache forms. While, ice pick, headaches are a bit less common, they are no less painful. Each of these is considered primary because they exist as the initial pain problem.
Tension Headaches
Tension Headaches are the most common form of headache. They may occur at any age. Tension headaches may be episodic (occurring less than 15 times in 30 days) or chronic (occurring 15 times or more in 30 days) in nature. Episodic tension headaches may last only 30 minutes or as long as a week. Chronic tension headaches may run the stretch of a few hours but are often continuous or reoccurring in nature.
- Possible Triggers: Elevated stress levels may trigger tension headaches in some individuals.
- Tension headaches do not bring nausea or vomiting. They will also not be brought on by intense physical activity. A dull aching pain with a feeling of a band placed tightly around the head is how sufferers describe tension headache pain.
Migraine Headaches
Migraine Headaches remain the second most common form of headache. Migraine headaches can be as short as a few hours or as long as a few days. They are usually reoccurring in nature.
- Regarding Possible Triggers: Each patient will have a different set of possible triggers for migraine pain. It may be beneficial for patients to consider hormonal changes, environmental factors including weather and lighting, medications, sleep patterns, food and beverage choices, and patterns of physical exertion.
- Paying attention to warning signs that will often occur prior to a migraine setting in becomes key in managing migraine pain. Warning signs may include flashes of light, emotional disturbances like depression/anxiety, blind spots, tingling sensations in the face or arms.
Cluster Headaches
Cluster Headaches (also known as neurovascular headaches) are called this because they often happen one after another in a short period of time. This type of headache can last for a few minutes or as long as a few hours. While cluster headaches are not considered life threatening, they are known to be one of the most painful types of headaches.
Cluster headaches often awake the sufferer from sleep. Pain may center around one eye, radiating to other parts of the head and through the neck area. Intense pain will be focused on the same side of the head. The same eye may experience redness, stuffiness, excessive tearing of the duct, and may droop. Sensitivity to light may only be present on one side.
- Cluster headaches are not often associated with direct triggers. Although, sufferers may note that existing pain experiences are intensified by alcohol consumption. Individuals who smoke may also be at a higher risk for developing cluster headaches.
- Direct causes are not known. However, patterns usually involve pain surfacing about the same time daily (or several times weekly), often shortly after one falls asleep. Pain often diminishes rapidly, leaving the sufferer exhausted (perhaps, in part, due to a repeated loss of sleep).
Ice Pick Headaches
Ice Pick Headaches may rapidly end or last for several days. Occurrences may seem random and unrelated to anything that the sufferer is actively doing at the time. However, it feels like an ice pick has been shoved into the head or face.
- Possible Triggers: This will vary by the individual and may be difficult to decipher. Sudden movements, stress and bright light are factors for some ice pick headache sufferers. Tension and migraine sufferers may also experience ice pick headaches.
- The debate remains: Can ice pick headaches develop as symptoms of disease? Here they are noted as primary due to the manner in which their pain is generated by the body. They are often left unexplained by a source outside of the structures of the head. Disease may take some blame for ice pick headache pain, but the exact source of the pain will often remain unclear.
A Few Secondary Headaches and What Causes Them
We often find a higher number of possible causes for secondary headaches. Trauma, disease, dehydration, influenza, stroke, environment, and personal choices may all play a direct role in the occurrence of secondary headaches. There is such a wide variety of potential secondary causes – underlying medical conditions, high blood pressure, anxiety/depression/PTSD, stress, blood clots, etc.
Sinus Headaches
Sinus Headaches are often listed with the top five commonly occurring headaches.
Sinus cavities are found inside of the forehead, cheekbones, and behind the bridge of the nose. This is where sinus pain and pressure are felt by sinus headache sufferers.
- A sinus headache is caused when the space that is meant to drain mucus becomes inflamed. This is due to a lack of proper drainage throughout the sinus cavities. Allergens can play a role in sinus complications.
- A fever may be present at some point during the inflammation. Pressure is built in this area as a result of the inflammation and insufficient mucus drainage causing pain. Chiropractic treatments can work to alleviate pressure in the sinus cavities.
Cervicogenic Headaches
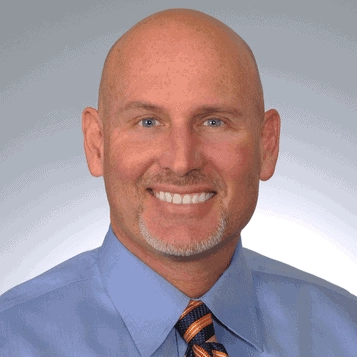
Cervicogenic Headaches are often difficult to distinguish from migraines. The difference is found in the source of the pain. This type of pain is caused by a cervical issue. It is considered referred pain. “The primary difference is that a migraine headache is rooted in the brain, and a cervicogenic headache is rooted in the cervical spine (neck) or base of the skull region.
Pain may last a few hours or more than a week. Considerations must be made for the reason for the pain. This type of headache will often come back until the source of the pain is resolved. Clinic HQ reads, “Many people find manipulative therapies such as Chiropractic, Osteopathy or Physiotherapy to be helpful in returning the neck, shoulder and upper back joints back to their healthy state.”
- Injury, whiplash, and arthritis may serve as an original source of the development of a cervical issue that leads to cervicogenic headaches. Placement of the head and neck during extended periods of time can also lead to cervicogenic head pain.
- Cervicogenic headaches may or may not include neck pain and a reduced range of motion. Pain is often most associated with one side of the head and neck area and may increase with certain movements.
Thunderclap Headaches
Thunderclap Headaches honor their name come on rapidly and may even take the sufferer by surprise. After about 60 seconds, a thunderclap will usually peak in its level of pain. Pain may occur anywhere in the head (and possibly in the back) and can last a few minutes or a whole week.
- Possible Triggers: Intense physical labor, encountering hot or cold water rapidly and certain drugs may act as triggers for some individuals. Causes may be related to infection in the brain, aneurysm, issues with arteries or blocked veins, spinal fluid leaking or other dangerous issues that need attention.
- It is also possible to experience nausea, vomiting, and a loss of consciousness with a thunderclap headache. This type of headache can be a sign of a severe and potentially fatal condition. Immediate medical attention must be sought to avoid risky complications.

Should I See a Doctor for My Headaches? How Soon?
Do we just need a good meal, water, and some rest? There are times when this is just not going to be sufficient. Three or more headaches within the span of one week would easily justify the need for meaningful medical attention. However, all head pain sufferers deserve healing.
Note: The following symptoms are considered serious and require immediate medical attention:
- Abrupt severe head pain can be the result of a serious condition. Seek medical attention.
- A loss of control within the body may be the sign of a serious condition. Headache pain may cause or be accompanied by other conditions (dizziness, unable to control feet or limbs, difficulty speaking, vomiting, loss of consciousness, or vision problems). Ensure that medical attention is acquired.
- Head injuries require immediate medical attention. Even if you hit your head or were in an accident a few days prior, headaches may begin to occur after the initial incident. Do not delay in seeking medical attention.
- Extreme, unexplained head pain (especially lasting 72 hours) needs attention. If pain causes alarm, seek immediate care.
Getting Rid of Headache Pain of All Types
When emergency related symptoms are not present but, a few basic steps may be found as beneficial. Try these options for headache relief:
- Find relaxing activities that help to minimize stress.
- Minimize light.
- Review food and beverages as consumed.
- Remember to drink plenty of clean water.
- Minimize muscular and spinal issues that may be related to headache pain with chiropractic adjustments or chiropractic massage.
We may often include many of these tasks in our regular activities. Consider each in a new light as you pursue what may be the best long-term course of action. Reviewing our overall health situation is always a good idea.
Better Health Chiropractic and Physical Rehab clinics welcome individuals seeking to solve the head pain puzzle. Chiropractic treatments work to facilitate nerve and brain health as well as promote general wellness within the body.